A systematic review of the literature conducted by a research team from the Istituto Zooprofilattico Sperimentale delle Venezie (IZSVe) has revealed that isolates of Salmonella enterica of animal origin harbour numerous genes conferring resistance to antimicrobials critically important for the treatment of human infections. Specifically, genes have been identified that encode resistance to quinolones and fluoroquinolones, particularly in poultry, followed by genes resistant to β-lactams and aminoglycosides, chiefly found in pigs. The study has been published in Research in Veterinary Science.
Antimicrobial resistance in Enterobacteriaceae according to a One Health approach

The antimicrobials administered to livestock and humans are often the same, or belong to the same drug class. An antimicrobial is defined as critically important when it is the sole, or one of limited available therapies used to treat severe bacterial infections that can be transmitted to humans from non-human sources, or that can acquire resistance genes from non-human sources. One inevitable side effect of their use is the spread of antimicrobial resistance. This phenomenon is exacerbated by inappropriate use of these drugs in human medicine and livestock production, fostering the spread of resistant bacteria in the environment
Antimicrobials, more commonly known as antibiotics, are essential for the treatment of bacterial infections in humans and animals. One inevitable side effect of their use is the spread of antimicrobial resistance. This phenomenon is exacerbated by inappropriate use of these drugs in human medicine and livestock production, fostering the spread of resistant bacteria in the environment.
The critical role of antimicrobials
The antimicrobials administered to livestock and humans are often the same, or belong to the same drug class. To maintain their therapeutic efficacy and limit the spread of resistant pathogens, the World Health Organisation (WHO) has conceived and published a list of critically important antimicrobials (CIA) for humans.
An antimicrobial is defined as critically important when it is the sole, or one of limited available therapies used to treat severe bacterial infections that can be transmitted to humans from non-human sources, or that can acquire resistance genes from non-human sources. The WHO classification ranks the following as critically important antimicrobials for humans:
- highest priority: cephalosporins (third, fourth and fifth generation), glycopeptides, macrolides and ketolides, polymyxins, and quinolones
- high priority: aminoglycosides, ansamycins, carbapenems and other penems, glycylcyclines, lipopeptides, monobactams, oxazolidinones, penicillins (natural, aminopenicillins, and antipseudomonas), derivatives of phosphonic acid, drugs used solely to treat tuberculosis or other mycobacterial diseases.
The spread of antimicrobial resistance in Enterobacteriaceae

Food systems are pivotal in the epidemiology of antimicrobial resistance. In fact, resistant bacteria can be transmitted to humans both through contact with animals, and through consumption of contaminated foods of animal origin. Furthermore, the increase in the occurrence and circulation of resistant bacteria in the environment may be due also to the transfer of genetic material among bacteria, which can exchange genes responsible for resistance mechanisms.
Food systems are pivotal in the epidemiology of antimicrobial resistance since they closely link humans and animals, suggesting that health is indeed one (One Health).
Resistant bacteria can be transmitted to humans both through contact with animals, and through consumption of contaminated foods of animal origin. Furthermore, the increase in the occurrence and circulation of resistant bacteria in the environment may be due also to the transfer of genetic material among bacteria, which can exchange genes responsible for resistance mechanisms.
Most antimicrobials currently used in veterinary practice are active mainly against Enterobacteriaceae, an important family of Gram negative bacteria, including Salmonella and Escherichia coli.
These bacteria are commonly present in the animal gut and are responsible for opportunistic infections in both humans and animals. They also pose a potential public health threat because they can develop and rapidly spread resistance genes, within both the same species and different species of bacteria.
Salmonella is an important member of Enterobacteriaceae by virtue of its pathogenicity, its noteworthy prevalence, and the frequent detection of resistance genes in various isolates.
Resistance genes in Salmonella enterica of animal origin: the IZSVe study
A research team at the Istituto Zooprofilattico Sperimentale delle Venezie (IZSVe) carried out a systematic qualitative review of the scientific literature to describe the distribution of genes conferring resistance to critically important antimicrobials in serovars of Salmonella enterica isolated from animals (cattle, pigs, and poultry), derived food products, and the surrounding environment. The study, which was part of a project funded by the Italian Ministry of Health (RC IZSVe 02/2016), was published in the journal, Research in Veterinary Science.
A comprehensive literature search was carried out on 31 scientific papers, selected after screening 7,955 articles which were identified in the scientific literature databases according to the research criteria. The systematic review revealed how isolates of Salmonella harboured many genetic determinants encoding resistance to treatment with critically important antimicrobials for humans. Genes conferring resistance to quinolones and fluoroquinolones – detected mainly in poultry – were the most prevalent, followed by genes with resistance to β-lactams and aminoglycosides, found mainly in pigs.
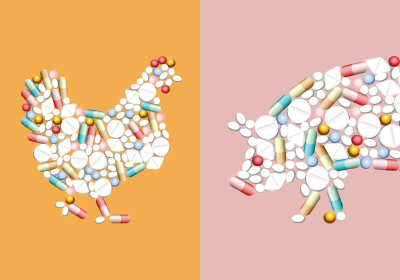
The systematic review revealed how isolates of Salmonella harboured many genetic determinants encoding resistance to treatment with critically important antimicrobials for humans. Genes conferring resistance to quinolones and fluoroquinolones – detected mainly in poultry – were the most prevalent, followed by genes with resistance to β-lactams and aminoglycosides, found mainly in pigs.
The use of specific classes of antimicrobials may explain the selection of resistance genes in zoonotic bacteria, such as Salmonella spp. Analysis of the genetic resistance profiles of each Salmonella isolate clearly shows that Salmonella Typhimurium and its monophasic variant – abundantly identified in the studied samples from swine and related sources – are characterized by the concurrent presence of numerous different resistance gene determinants. These enable the bacterium and its variant to resist a broad spectrum of antibiotics, particularly β-lactams and aminoglycosides.
In the samples of poultry and derived foods, analysis of the behaviour of Salmonella Infantis and Salmonella Enteriditis – variants typically isolated in poultry – yielded a different picture. S. Enteriditis tends to harbour resistance genes against quinolones/ fluoroquinolones or against β-lactams, whereas S. Infantis harbours resistance determinants against aminoglycosides or cephalosporins.
The presence of genes conferring resistance to antimicrobials appears to be much less widespread among cattle. What this finding suggests, nonetheless, is that the scientific evidence available for this production sector is currently incomplete.
The importance of the One Health approach
These findings confirm the need for a commitment at the European level to implement diagnostic and therapeutic approaches promoting the prudent use of antimicrobials in human medicine and livestock production. Despite growing attention to antimicrobial resistance in animal production, only few European monitoring programmes are currently in place to advance the study of the relationship between antimicrobial consumption and the transmission of resistance genes.
The fight against antimicrobial resistance on the part of veterinary medicine, the livestock sector, and health authorities must continue. Future intervention strategies must be governed more and more by the best available scientific evidence, of the type published in this paper.
Read the scientific article in Research in Veterinary Science »






